The development of drugs capable of attacking HIV at different points of its life cycle has completely transformed HIV treatment, with infected patients being able to live nearly as long as healthy individuals
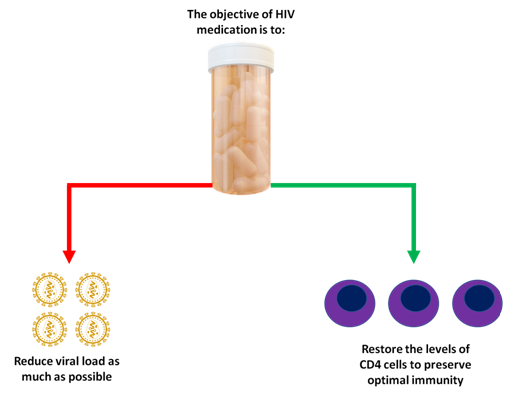
The goal of HIV treatment is to reduce the amount of virus (viral load) in the body, and to increase the number of CD4 cells in order to sustain a strong immune system against infectious microorganisms.
Effective management of HIV infection is possible with HAART (highly active antiretroviral therapy), in which a combination of several drugs is used to prevent HIV from replicating, reducing the risk of disease transmission and restoring immune system function.
But why do we need to use so many drugs?
This is because HIV mutates so rapidly that if only one drug was given, the virus would become resistant to the treatment super quickly, allowing the disease to potentially progress into AIDS. So by using several drug classes, the virus would have to undergo multiple mutations to develop resistance; and this is very unlikely to happen.
Currently, we have 4 drug classes that inhibit HIV replication at different points of its life cycle. They are:
· Fusion and chemokine receptor inhibitors
· Reverse transcriptase inhibitors
· Integrase inhibitors
· Protease inhibitors
When HIV infects an individual, the virus circulates in the bloodstream and uses CD4 T helper cells to replicate. In order to achieve this, the virus employs several highly specific proteins and enzymes; many of which can be targeted with HIV drugs.
So now, let’s dive into the HIV life cycle and examine how the different drugs attack the virus.
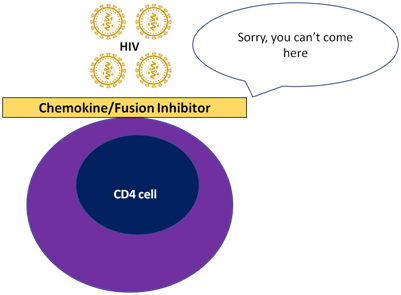
In order to gain access into the cell, HIV uses the membrane proteins (gp41 and gp120) to interact with the receptor CD4 and the co-receptor CCR5 on the surface of T helper cells. When this occurs, HIV is able to deceive the cell and release its genetic content.
[Fusion and chemokine receptor inhibitors block the CD4 receptor and CCR5 co-receptors, preventing the virus from entering into T helper cells]
Once HIV has entered the cell, the first thing it does is to modify its genetic material using the enzyme reverse transcriptase.
Do you know why it does this?
You see, our genetic material is found in chromosomes as double stranded DNA, whereas HIV has its genetic material in the form of single stranded RNA. So, by using reverse transcriptase, HIV converts its RNA into complementary DNA.
[Reverse transcriptase inhibitors block the actions of reverse transcriptase and prevent the virus from changing its genetic material into DNA]
After converting its genetic material into double stranded DNA, HIV uses an enzyme known as integrase.
As you can probably guess from its name, integrase inserts and integrates the viral DNA into the host cell genome. It is an impressive enzyme that zips a hole into our DNA, and then adds the viral genetic code into our cells.
Unfortunately, CD4 cells don’t realise when that they are hijacked; meaning that when they process their DNA to make proteins, they will actually produce HIV viral proteins!
[Integrase strand transfer inhibitors inhibit the actions of the integrase enzyme, blocking the integration of viral DNA into the genome of CD4 cells]

Even after the replication machinery of CD4 cells makes viral particles, HIV is still not ready and must assemble itself using yet another enzyme: protease.
Protease is essentially an organiser that gathers all the viral particles hanging around the cell, assembling a full mature HIV virus that is then ready to attack more CD4 cells.
[Protease inhibitors deactivate viral protease and halt the maturation of HIV. With these drugs, viral particles are still produced, but they are completely harmless and non-infectious]
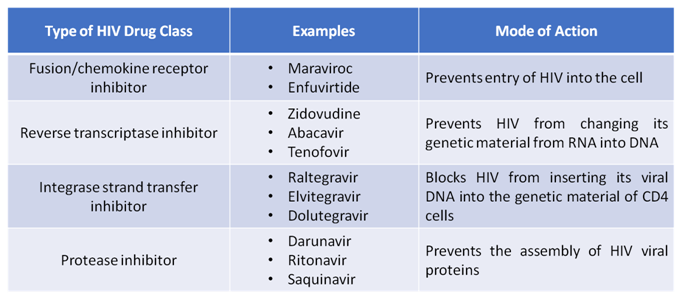
For each antiretroviral class, there are multiple drugs that have been developed over the last 30 years. Newer HIV drugs are more effective, safer and resistant to mutations.
But developing drugs is not always about effectiveness and tolerability, but also about making life easier for patients.
In the past, patients had to take multiple HIV pills each day, but now we have entered the stage where we have single tablet regimens or STRs.
STRs contain multiple HIV drug classes within a single pill, meaning that patients only have to take one tablet, once daily.
The simplicity of taking STRs have been shown to boost adherence in HIV patients, something which is critical in reduce the risk of HIV transmission and the emergence of viral mutations.
With the wide range of effective, safe and simple HIV medications that are available, we have the means to eliminate AIDS within this century.










