Don’t miss the key findings of the first study which assessed the relationship between patient blood group and COVID-19.
With the rapid growth in the number of SARS-CoV-2 infections and COVID-19 fatalities, there is an urgent need to develop biomarkers that may help us to identify the most vulnerable patients.
The use of blood group as a biomarker may be useful for COVID-19 because there is evidence that in other viral illnesses (e.g. Hepatitis B) having a certain blood group influences risk of disease.
Knowing this, a group of researchers collected data from a Chinese hospital in a total of 1,775 patients infected with SARS-CoV-2.
The researchers used blood group records from 3,694 non-infected patients from Wuhan to act as a control. In studies we always need a control to compare measurements, otherwise what you find loses credibility.
Now, let’s see what they found!
The proportion of blood group A patients with COVID-19 was significantly higher compared to non-infected people (37.8% vs. 32.2%).
In contrast, the proportion of blood group O patients with COVID-19 was significantly lower compared to non-infected individuals (25.8% vs. 33.8%).
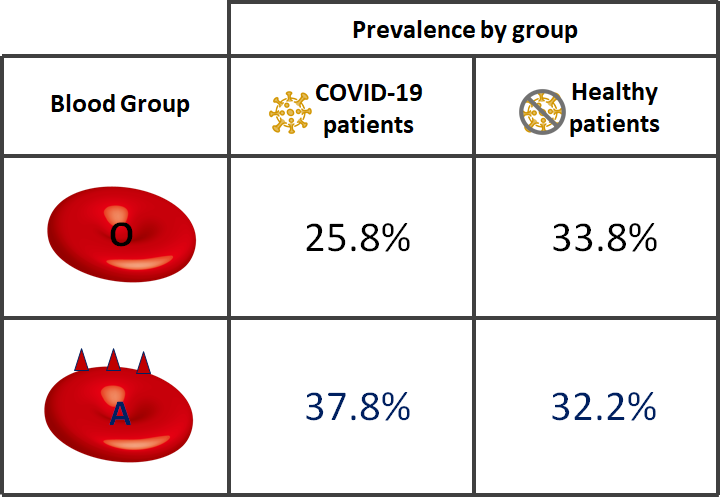
These results suggest that patients with blood group A may be more susceptible to developing COVID-19 when infected by SARS-CoV-2 compared to those with blood group O.
However, you might be questioning whether patients who had died influenced these findings…
Fortunately, the researchers thought of this and included blood group records from 206 patients who had died of COVID-19.
Again, similar trends applied…
Blood group A was associated with a 48% higher risk of death compared to the other blood groups. Whereas, blood group O was associated with a 37% lower risk compared to non-O blood groups.
This study confirms previous findings in SARS-CoV (a very similar virus to the current coronavirus), in which it was revealed that medical staff in Hong Kong were less likely to be infected if they were blood group O.
Although both studies are only showing an association, there is in fact science to back up these trends.
Individuals that are blood group O produce anti-A antibodies against the red blood cells of people with blood group A. On the other hand, individuals with blood group A don’t produce these antibodies as they would destroy their own blood cells!
Surprisingly it seems that these anti-A antibodies don’t just target foreign red blood cells, but they appear capable of inactivating the SARS-CoV virus too!
Due to the similarity between SARS-CoV and SARS-CoV-2, these findings may explain why fewer individuals with blood group O had COVID-19.
You see, both these viruses use the S protein to enter into human cells which express the ACE2 receptor. The anti-A antibodies from individuals with blood group O blocked the binding of viral protein S to the ACE2 receptor in human cells, consequently blocking its entry.
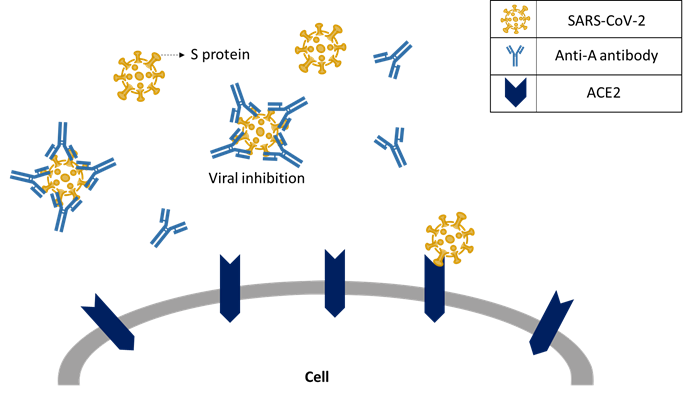
Please note that being blood group O does not grant you automatic protection against the virus. Nevertheless, the presence of anti-blood antibodies may give you a slight advantage if you are infected by SARS-CoV-2, compared with someone who is blood group A.
Once more studies confirm these trends, we will probably begin to use blood group information as a biomarker to quantify COVID-19 risk in patients.
For now, everyone should be as cautious as they can, regardless of what blood group they may be.